Bilateral Salpingo-Oophorectomy and Hysterectomy: Comprehensive Insights into Women's Health Procedures
In the realm of women's health, understanding the complexities of various surgical procedures is vital. Among these, bilateral salpingo-oophorectomy and hysterectomy stand out as significant interventions for addressing various gynecological conditions. This article delves deep into these procedures, the indications for their performance, their benefits, and what patients can expect during recovery.
The Importance of Women’s Health
Women's health encompasses a wide range of issues, from reproductive health to hormonal balance. As clinical awareness evolves, more women are seeking surgical options that provide answers to persistent health challenges.
What is Bilateral Salpingo-Oophorectomy?
A bilateral salpingo-oophorectomy (BSO) is a surgical procedure that involves the removal of both the ovaries and fallopian tubes. This procedure is commonly performed alongside a hysterectomy, but it can also be carried out independently in certain circumstances.
Indications for Bilateral Salpingo-Oophorectomy
- Ovarian Cancer: One of the primary reasons for performing a BSO is the presence of ovarian cancer, particularly when diagnosed at an advanced stage.
- Severe Endometriosis: In cases where endometriosis causes significant pain and dysfunction, BSO may be considered to alleviate symptoms.
- Genetic Predispositions: Women with BRCA1 or BRCA2 gene mutations may opt for BSO to reduce their risk of developing breast or ovarian cancer.
- As Part of a Hysterectomy: When a woman undergoes a hysterectomy due to fibroids or other issues, BSO may be recommended concomitantly as a preventive measure.
Benefits of Bilateral Salpingo-Oophorectomy
The benefits of undergoing a bilateral salpingo-oophorectomy can be profound, depending on the underlying condition being addressed:
- Risk Reduction: For women at high risk for ovarian or breast cancer, BSO can significantly reduce the likelihood of these cancers developing.
- Symptom Relief: Many women report a marked improvement in symptoms related to endometriosis or other gynecological conditions once the procedure is performed.
- Improved Quality of Life: Patients often experience an enhanced quality of life following the surgery, free from the pain and complications associated with their previous conditions.
What is a Hysterectomy?
A hysterectomy is a surgical procedure to remove the uterus. Depending on the clinical need, a hysterectomy can be total (removing the uterus and cervix) or partial (removing only the uterus, leaving the cervix intact).
Reasons for a Hysterectomy
Several indications may lead a healthcare provider to recommend a hysterectomy:
- Uterine Fibroids: Noncancerous growths in the uterus can cause a range of symptoms including heavy bleeding and pelvic pain.
- Endometriosis: Severe endometriosis that does not respond to other treatments may necessitate a hysterectomy.
- Uterine Prolapse: A condition where the uterus descends into the vaginal canal, often leading to discomfort and urinary issues.
- Cancer: Hysterectomy may be required to treat certain cancers of the uterus, cervix, or endometrium.
Benefits of Hysterectomy
The decision to have a hysterectomy can lead to various benefits for women:
- Relief from Symptoms: Many women experience significant symptom relief following a hysterectomy, particularly those suffering from fibroids or endometriosis.
- Reduced Risk of Certain Cancers: By removing the uterus, the risk of developing uterine cancer is eliminated.
- Improved Quality of Life: Many report a marked improvement in overall well-being post-surgery.
The Procedure: What to Expect
Preparation for Surgery
Prior to surgery, thorough preparations are essential. Your healthcare team will:
- Conduct pre-operative assessments: This includes discussing your medical history and performing necessary examinations.
- Review any medications: It’s crucial to discuss all medications and supplements with your doctor.
- Arrange for post-operative care: Planning for recovery assistance is vital for a smooth transition post-surgery.
The Surgical Procedure
The type of surgery may depend on multiple factors, including the reason for surgery and individual patient considerations. Techniques can include:
- Open Surgery: Involves larger incisions and longer recovery times.
- Laparoscopic Surgery: Minimally invasive with smaller incisions, usually resulting in quicker recovery times.
- Robotic Surgery: A newer technique that allows for precision and reduced recovery time.
Recovery After Bilateral Salpingo-Oophorectomy and Hysterectomy
Post-operative recovery is a crucial phase that should not be overlooked. Here is what women can typically expect:
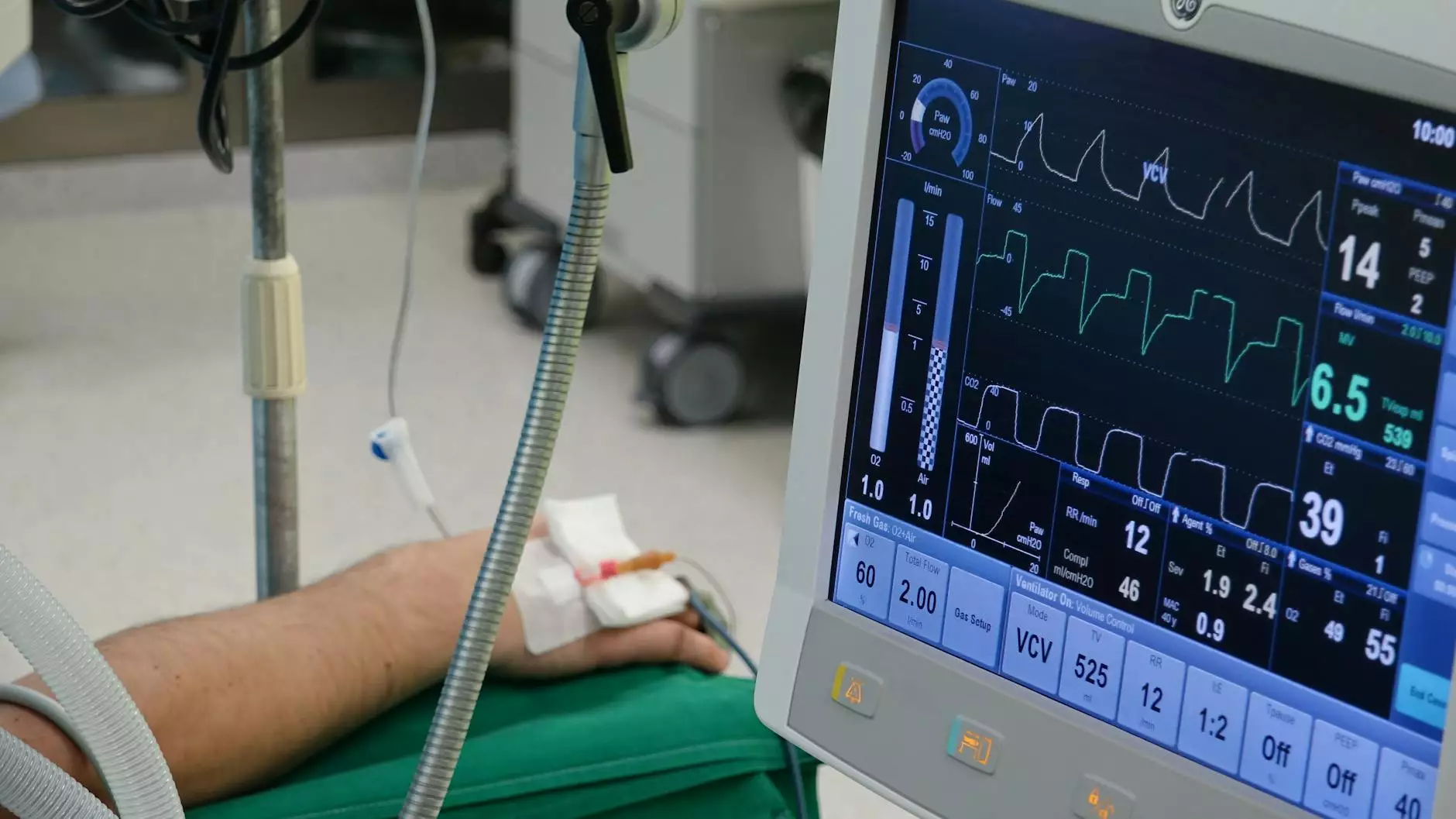
Immediate Post-Operative Care
- Hospital Stay: Depending on the procedure, patients may stay in the hospital for 1-3 days.
- Pain Management: Doctors will prescribe pain relief to help ease recovery.
- Activity Restrictions: Patients will often be advised to limit physical activity for a set period.
Long-Term Recovery
The long-term recovery process may vary. Important considerations include:
- Follow-Up Appointments: Regular follow-ups are essential to monitor healing and address any concerns.
- Manage Hormonal Changes: BSO may induce menopause, necessitating hormone replacement therapy (if applicable).
- Emotional Support: It’s important to seek emotional and psychological support during the adjustment period.
Choosing the Right Healthcare Provider
When considering a bilateral salpingo-oophorectomy or hysterectomy, choosing a knowledgeable and compassionate healthcare provider is essential. At Dr. Seckin's practice, we prioritize patient education, individual care plans, and comprehensive support throughout each step of the process.
Why Choose Dr. Seckin?
- Expertise: A wealth of experience in women’s health and surgical interventions.
- Patient-Centered Care: Focus on tailored treatment plans to best serve each patient’s unique needs.
- Supportive Environment: Emphasis on providing emotional and physical support throughout the surgical journey.
Conclusion
In conclusion, understanding bilateral salpingo-oophorectomy and hysterectomy is crucial for women facing various health challenges. These procedures can lead to significant improvements in quality of life and health outcomes. If you are considering these surgical options, consult with Dr. Seckin to ensure that your questions are answered and your unique health needs are addressed. Women deserve comprehensive care and support during their health journeys, and you are not alone in this process.
For more information or to schedule a consultation, please visit drseckin.com.